Physician–Patient Encounters in the Swedish Context
Medical students are told that they must be empathetic. (---) But, how do you understand another person? The medical students are told that they must ask about the person’s ideas and fears. A patient once said, “I’m not a jukebox where you push a button and then I sing”. (Seeberger 2010: 82, 98, authors’ translation)
In her novel The Shameless Curiosity (Den skamlösa nyfikenheten), the Swedish physician and writer Astrid Seeberger (2010) reflects on encounters between care providers and care seekers. As the quote indicates, while physicians are trained to take into account patients’ feelings and subjective experiences, patients may still feel reluctant to do so. Based on her many years of professional experience, throughout the novel Seeberger (2010) emphasizes the importance of understanding physician–patient encounters not only as medical consultations, but also as building a relationship embedded in sociocultural structures and thus permeated with specific views and expectations of parties involved.
A broad scientific literature discusses that political endorsement of individual responsibility and free choice affect self-care practices (Gabe, Harley & Calnan 2015; Michailakis & Schirmer 2010). Previous studies have noted that health consumerism increasingly becomes everyday parlance (Henderson & Petersen 2002). This, in turn, presents challenges to the authority of care providers (Gabriels & Moerenhout 2018; Liu & Lundin 2020). One such challenge is how physicians can provide care and engage with care seekers. In medical anthropology, scholars such as Kleinman and Mol argue that a focus on care is essential in the practice of medicine (Kleinman 2013; Mol 2008). Literature on medical education also identifies the benefits of physician empathy in improving care service quality (Derksen, Bensing & Lagro-Jassen 2013). These studies cohere with the shift in healthcare models in Sweden and elsewhere, from cure-oriented to patient-oriented, where the latter calls for integration of care seekers’ illness experiences and needs into physician–patient encounters (Epstein & Street 2011; SOU 1997:154).
Alongside these shifting relationships between care providers and care seekers there have been societal changes with significant implications for the pharmaceutical market, and thus also for individuals. In Sweden where data from this article was obtained, a major change was the deregulation of the Swedish state-owned pharmacy, Apoteket AB, which in 2009 was replaced by a liberal market structure and multiple private owners. In recent years, pharmaceutical services have increasingly become digitally accessible for Swedish residents (Statista 2020). Digital platforms also provide spaces for people to share health information and care seeking experiences (Lupton 2018). Simultaneously, they facilitate easy access to medicines from all parts of the world whose quality can be questionable (Mackey & Nayyar 2016). Against this background, access to medicines that falls between legal and illegal domains is identified by international police authorities and health organizations as a potential risk to individual and public health (Hall & Antonopoulos 2016; World Health Organization 2017). Such an in-between space has grown partly out of disparate regulations applied in different countries or a lack of clearly articulated regulations in a given jurisdiction (Lavorgna 2021). We refer to this blurred area between legal and illegal domains as grey zones (Nordstrom 2007).
Apart from potential medical risks, medicine access in grey zones is relevant from a social standpoint. The consequences for individuals who, intentionally or otherwise, make purchases in grey zones can be far-reaching within the Swedish context. By Swedish law, care seekers are entitled formal health services and insurances if they acquire medications through authorized healthcare providers. Purchases outside the formal healthcare that may lead to unwanted medical effects are not covered by national insurance, meaning that individuals must take full responsibility for any outcomes. In other words, it is important for care seekers to be aware of what applies to medicine purchases. It is also essential for care providers to gain knowledge about medicine access in grey zones in order to engage with care seekers in a meaningful way.
Linking back to Seeberger’s (2010) reflection on physician empathy and the challenges care providers face to support safe medicine access, the aim of this article is twofold. Firstly, we want to advance sociocultural analyses that explore how the interaction between physicians and care seekers is embedded in a web of social relations and material resources. Here we address a number of questions. How do care seekers and physicians respectively perceive medicine access in grey zones? How do their views affect physician–patient encounters? Secondly, we seek to contribute knowledge that can be implemented in healthcare.
In what follows, we first present the subject of medicine access in grey zones. The potential risks posed by medicines circulating in grey zones point to an urgent need to understand what constitutes good care and what is required to build an engaging physician–patient relationship. Next, we discuss the materialities of medicines in order to conceptualize physician–patient relationships as embedded in societal structures. This is followed by a presentation of methods and materials. Our team has an interdisciplinary profile, with researchers from the humanities, social sciences, and medicine. We share an interest in care services and physician–patient relationships. Materials were collected from multiple sources, both online and offline in Sweden. We bricolage the various types of data to identify the diverging views held by Swedish physicians and care seekers. Subsequently, we demonstrate care seekers’ attitudes towards medicine access in grey zones in relation to their experiences of formal healthcare. We then turn to physicians and discuss their knowledge and perceptions of medicine access in grey zones. Finally, by drawing on our analyses we suggest conceptual tools to support physicians when interacting with care seekers in medical consultations.
Medicine Access in Grey Zones
Access to the internet has opened up a global market for purchasing medicines within and beyond legal domains (Hall & Antonopoulos 2016). To regulate the online pharmaceutical market, all authorized internet pharmacies operating within the European Union must display a logo on their homepage.1 Our previous findings (Liu & Lundin 2020), however, show that people are rarely observant of whether the sites they visit are certified or not.
To address the issue of medicine access in grey zones and potential health risks related to them, the World Health Organization proposes the term “substandard and falsified medical products” (hereafter, falsified medicines), to refer to medicines that do not meet quality standards or deliberately misrepresent their composition or sources (World Health Organization 2017). Stakeholders, including governmental agencies and nonprofit organizations such as the Pharmaceutical Security Institute, look upon macrolevel interventions to limit the spread of these falsified medicines. These measures include harmonizing international legal frameworks and innovating tracking technologies (Attaran 2015; Naughton 2019; Hamilton et al. 2016). The dominant discourse on this subject tends to victimize care seekers purchasing medicines through alternative channels (Liu & Lundin 2016). Yet empirical studies, not least by criminologists, show a complex situation. Some care seekers intentionally transgress legal boundaries, while many others are not aware that it may be illegal, both of which potentially lead to unwanted or unexpected medical side effects (Lavorgna 2021; Hall & Antonopoulos 2016; Sugiura 2018).
A small but steadily growing body of research focus on the specificities of local markets and everyday care practices (Hornberger 2019; Baxerres & Le Hesran 2011; Hamill et al. 2019). It highlights ambiguities in the categories of falsified or substandard medicines and suggests that these ambiguities need to be examined by situating medicine access in specific social contexts (Kingori & Gerrets 2019: 380). Medicines in this research area are perceived as objects whose efficacy is both therapeutic and social. Hence, the boundary between good and bad quality, legal and illegal status, is inherently fuzzy (Nordstrom 2007). Medicine quality is contingent upon local regulations, healthcare structures and sociocultural interpretations of medicines (Quet 2017). Understanding the issue of medicine access in grey zones thus requires more than simply examining biomedical standards or legal requirements. It requires more knowledge of how the different parties involved in healthcare negotiate their respective views on medicines and care practices.
Materialities of Medicines
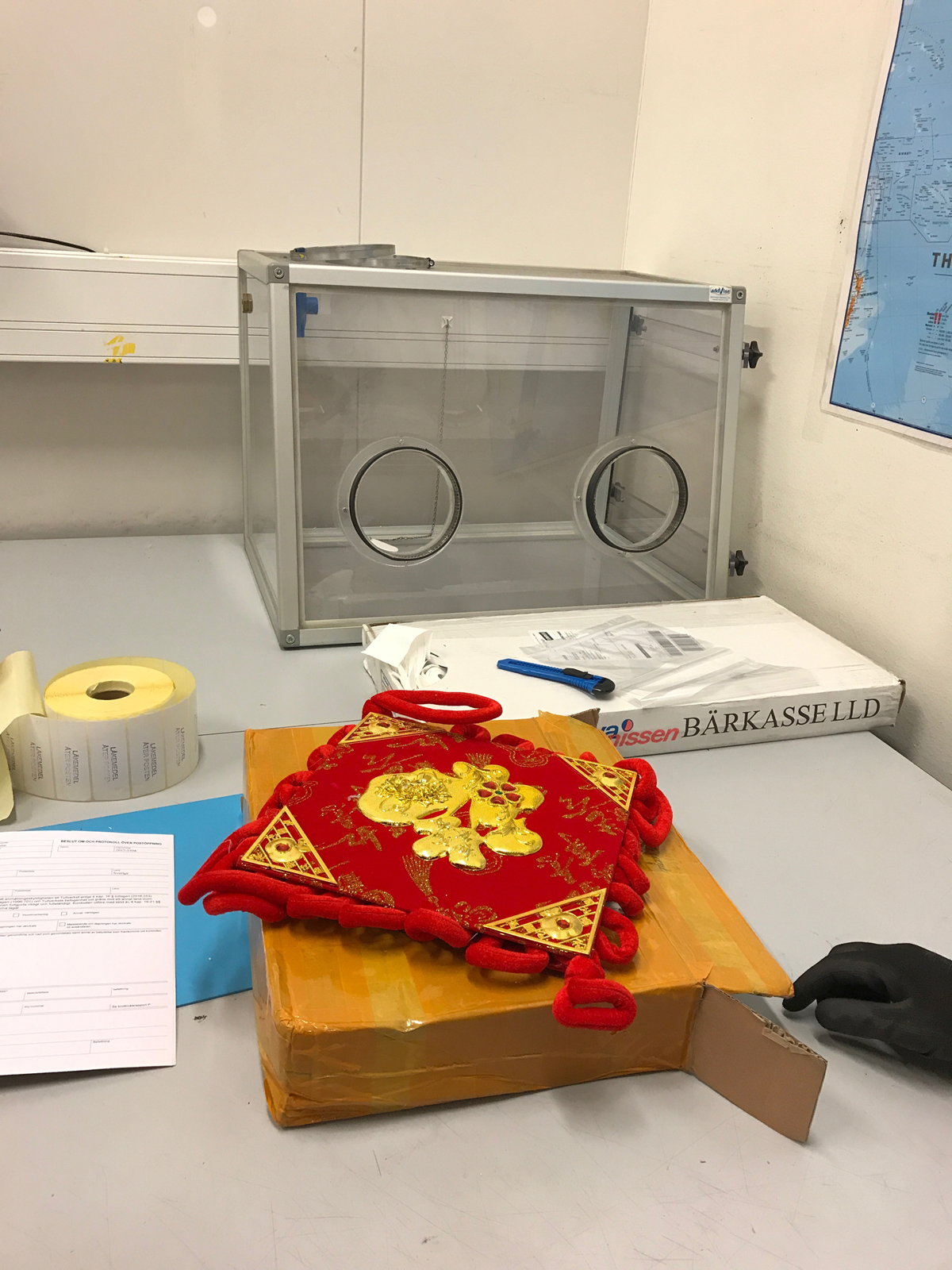
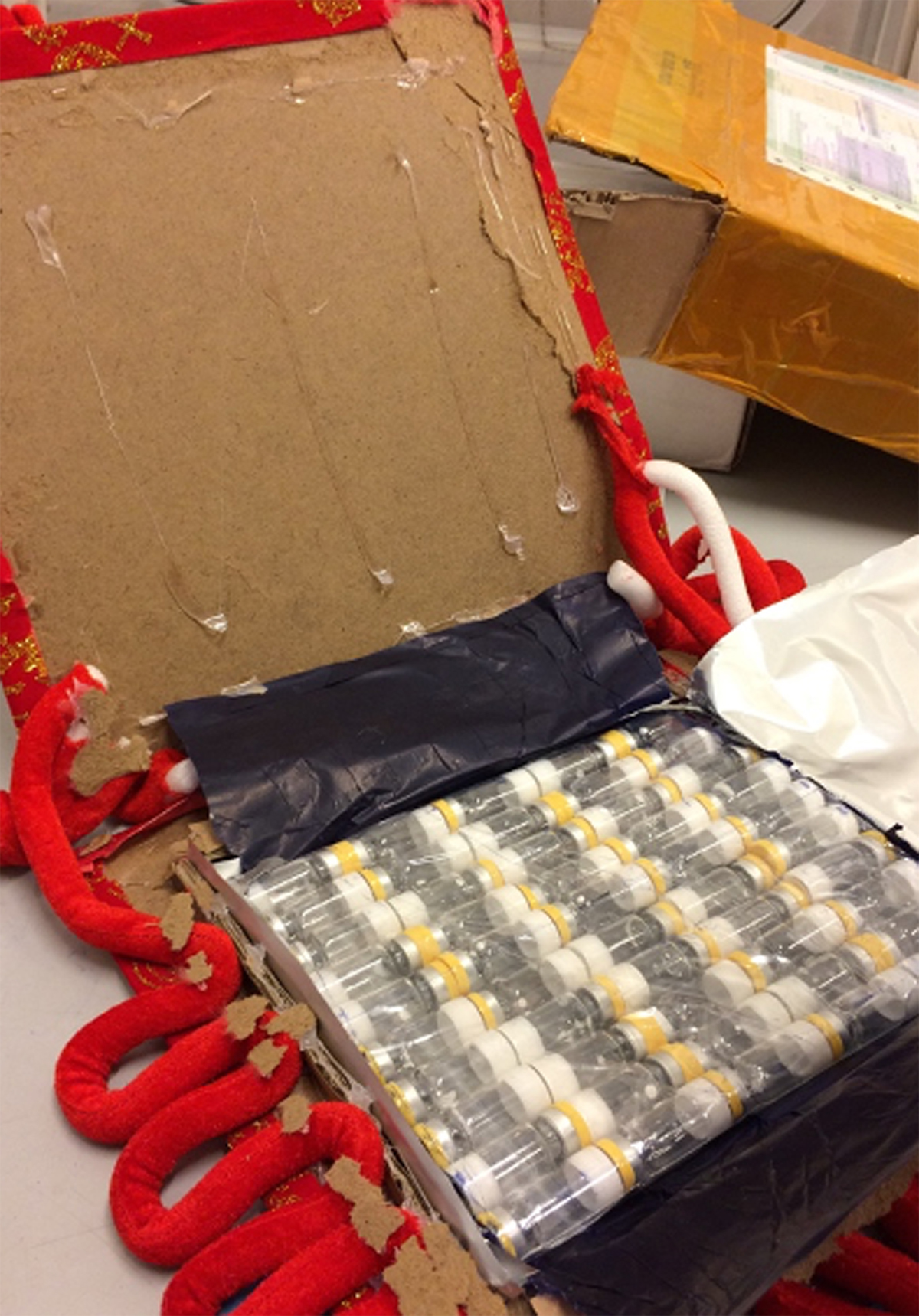
To study physician–patient relationships in connection with medicine access in grey zones, we utilize the concept of the materialities of things and take a relational approach to argue that medicine access is shaped by specific social and material configurations. In the seminal work by Appadurai (1986), things acquire meanings when moving through different regimes of value. Thus medicines, genuine or falsified, can be viewed as objects whose values do not simply lie in their therapeutic quality, but in the social relations established through their movement and interaction with people in the society (Whyte, van der Geest & Hardon 2002). In September 2017 we conducted participant observation at a postal checkpoint at Arlanda International Airport, in collaboration with Swedish Customs (Liu & Lundin 2017). It was part of the International Criminal Police Organization’s annual operation Pangea, targeting the online circulation of illicit pharmaceuticals (Interpol 2017). We followed Swedish Customs officials who identified several postal packages disguised as elaborate decorations while containing illegal medical products sent from abroad (see Figures 1 and 2). These packages were only a tiny fraction of the entire seizure during the operation Pangea in 2017 (Interpol 2017). This field observation allowed us to empirically capture one phase in the social life of falsified medicines as material objects, namely their movement from producers to users. It also inspired us to utilize Appadurai’s theory of the social lives of things in our analysis.
In the literature, there are many examples showing the social life of medicines. To illustrate, one study of a poor area in the Philippines examined how women scrape together their last pennies to buy medicines for their sick children (Whyte, van der Geest & Hardon 2002). Not only should the medications heal the children, but by purchasing medicines, the mothers demonstrate that they are responsible and caring parents (Whyte, van der Geest & Hardon 2002). Another example, illustrated in Coderey’s (2019) research in Western Myanmar, reveals that consuming Western medicines is perceived as a way to participate in an out-of-reach “modern” world. Both above-mentioned studies indicate that there are social and moral incentives underpinning the consumption of medicines beyond merely perceived cures for health problems.
The metaphor of things with a social life (cf. above) has been useful in understanding how objects in motion acquire values. We also find this metaphor fruitful in highlighting the relational and emergent aspects of things. Ingold (2012: 436) argues that things are the “gathering of materials in movement”. They are the results of negotiated processes between matter and form during which a wide range of social and material resources are mobilized (Ingold 2012). Medicines, therefore, can be viewed as fluid objects (Hardon & Sanabria 2017), whose quality and efficacy are subject to sociomaterial configurations (Sachs 2006; Quet 2017). Combining Appadurai’s social lives of things with Ingold’s materialities as processual, we view medicine access as a situated everyday practice at the intersection of liberalized and globalized market structures and changing relations between care seekers and care providers. Care is not a product that can simply be given or received, but a practice enacted in a web of sociomaterial relations (Mol 2008). In this regard, a relational approach with an emphasis on materialities as charged with negotiations, helps to examine how different perceptions of care and medicines held by care seekers and physicians affect medical encounters.
Methods and Material
Cultural studies have a long tradition of methodological eclecticism (Marcus 1995; Ehn, Löfgren & Wilk 2016: 132). We collected data through bricolage in which qualitative material is put in dialogue with statistical data (Lundin & Idvall 2003; Teddlie & Tashakkori 2012; Wiszmeg et al. 2012). Such an approach has allowed us to move between fields in virtual and physical spaces. We follow Krieg, Berning and Hardon’s (2017) idea that qualitative and quantitative data are symbiotically connected through the concept of “field groundedness”, and that online and offline should not be distinguished from each other to gain deeper knowledge (ibid.). This is in line with Burrell’s (2009) argument that a field site is a network of interconnected locations across digital and physical space. This implies that the researcher strives to recreate this network through a well-considered bricolage of empirical materials from various sources.
Our empirical material consists of responses from two main groups in Sweden: physicians and care seekers. The first group was approached through a web survey designed by our project team (Funestrand et al. 2019). The survey was conducted by the Swedish market research institute Kantar Sifo. It was an online questionnaire with a mixture of multiple-choice questions and open-ended ones. We collected anonymous responses from 100 general practitioners (GP) and 100 physicians in emergency care (EP). The group of GPs consisted of 60 percent males and 40 percent females. Their median age was 60 years. The group of EPs consisted of 68 percent males and 32 percent females with a median age of 58 years. These physicians were asked about their knowledge of falsified medicines and if they had experiences of patients consuming any such medical products. Responses to multiple-choice questions were analysed statistically. The open-ended questions offered room for respondents’ own comments and provided opportunities for interpretive analyses.
Responses from care seekers were collected at multiple sites. Most of the data was obtained through an online survey designed by the authors with assistance from the Folk Life Archive at Lund University. The questions aimed at examining thoughts regarding care-seeking experiences and the purchase of medicines, especially those that should be purchased only with prescriptions in authorized pharmacies in Sweden. We used the open-source survey tool LimeSurvey. In total, 155 answers were collected: 72 percent from women, 27 percent from men, and 1 percent from persons who did not want to indicate their gender. Their median age was 45 years old. Similar to the questionnaire for physicians, the survey for care seekers offered a free text space for comments.
Considering the rise of digital health practices, in which people increasingly search for and share health-related information (Maslen & Lupton 2019), we also followed discussion threads about medicine access on the Swedish chat forums Flashback and Familjeliv (Liu 2019; Lundin 2019). These digital forums provide free spaces for anyone who wants to start or participate in discussions on nearly any topic from public policies to very personal and private issues. Participants have the option to disclose or anonymize their identities. And all discussion threads are openly available to forum users and non-users. Search words included “buy medicines” (köpa mediciner), “buy without prescriptions” (köpa utan recept), and “internet pharmacies” (internetapotek) to identify relevant discussions. The collected data aimed to provide a background understanding on what experiences and opinions people shared with peers. We did non-participant observation by reading how thread contributors interacted with one another and how various dynamics were created. Additional empirical materials were derived from participant observation in an urban primary care centre, in which fieldnotes were written by one of the authors, who also worked as a physician (Troein 2020). These fieldnotes were originally produced as completely anonymized case studies and for educational purposes in physician training.
Quotations cited in this article are from all the above-mentioned sources, including the surveys and field observation at multiple sites.2 No responses contained identifiable personal data. To distinguish the respondents in the two surveys, we refer to respondents in the Sifo survey as care providers or physician-respondents, and respondents from the LimeSurvey as care seekers or lay respondents. The term patient is used when it appears in original quotes.
What Care Seekers Said
In multicultural societies such as Sweden, physicians and care seekers do not always have a shared understanding of sickness or therapy practices, which may lead to disagreements on medications (Wachtler, Brorsson & Troein 2006). With increasing acknowledgement of the value of lay knowledge, traditionally paternalistic physician–patient relationships are under pressure to change (Fioretos, Hansson & Nilsson 2013). Taking these already identified frictions as a starting point, in this section we discuss how care seekers experience their encounters with care providers with regard to procurement of medicines. In health policies, care seekers are addressed as customers and encouraged to actively participate in their treatment (Irvine 2002). Our material, however, suggests that lay respondents experienced physicians as medicinal gatekeepers, making it difficult for care seekers to actively participate. One lay respondent wrote:
Healthcare acts paternalistically and I often feel very diminished in such situations when you are not trusted and especially in mental healthcare (…) they do not trust that I can handle a large package of sleeping pills without taking an overdose.
In this quote the respondent felt diminished by not being trusted by physicians. Accordingly, her attitude towards medical consultations was hesitant. Similarly, one lay respondent said that he preferred not going to physicians because “they do not take me seriously”. Another sought help outside formal healthcare because “you don’t get any help but are sent back and forth and you are ignored”. Mol (2008) has demonstrated that care seekers’ dissatisfaction with healthcare is not always about whether they are provided with treatment alternatives, but is more tightly connected to feelings of being abandoned or neglected by care providers. Our empirical material supports this observation. When discussing access to medicines, many respondents acknowledged physicians’ expertise to make well-grounded diagnoses. At the same time, they also expressed willingness to share the responsibility with physicians, rather than to completely rely on physicians or, alternately, shoulder the full responsibility for their own care. When care seekers sensed that their illness experiences were not respected or that care providers did not actively participate in this process, medical consultations lost their meaning and value.
Although several lay respondents did not recall any unpleasant encounters with physicians, some of them still preferred to self-medicate in the first place because they found it more efficient and convenient. One respondent revealed, “I find a lot of information out there (…) I would probably shop on the first website that offers what I want”. This practice of looking for easy shopping and alternative medical opinions echoed in our material collected from the online chat forums (Liu 2019; Lundin 2019). One person on the internet forum Flashback asked for advice:
Does anyone know anything about Valium or Stesolid [sedative drugs that must be prescribed by physicians]? Is there anyone who has tested [them] and can compare [them] with other diazepam and rate? I’m seriously considering buying some to test! Grateful for good answers.
The discussion threads contained suggestions from many people who claimed to be knowledgeable and acted as advisors. One of them responded that “Blue Roche valium and e.g. stesolid 10 mg both contain the right amount of diazepam”. This person then continued by stating that “there are a plethora of various diazepam preparations of unknown origin containing an unknown amount of diazepam. There are of course other serious diazepam products but valium and stesolid are the most well-known and if you get them you have the real deal.” This discourse on the internet cohered well with lay respondents’ statements. One person described: “you can get tips – and it is somewhat like going to the physician”. Another wrote:
Unlike the official information pages such as 1177 [Swedish national digital healthcare information hub] or the Medical Products Agency, you can through the forum [Flashback] communicate with people who have tried just what you are interested in and know how it worked for them (…), and then, all of a sudden you become like a physician who has 20 testimonies from a certain drug.
The above-presented quotes from the survey and chat forums indicate that there are self-claimed medical experts on these digital platforms who willingly offer advice, suggestions, even diagnoses to other forum members. In these forums we identified digitally engaged care seekers (Lupton 2014) who actively sought medical support. This contrasts with the prevailing perception within the literature on falsified medicines that care seekers purchasing medicines from alternative channels are merely victims (Liu & Lundin 2020). Furthermore, it is interesting that thread followers rarely showed any doubts about the honesty, expertise, or authority of these self-appointed medical experts (Lundin & Liu 2019). To some extent, this can be interpreted as a push-and-pull effect. On the one hand, care seekers experience their relationship with physicians as unequal, with feelings of being pushed away. On the other hand, care seekers can receive rather active and prompt responses from peers on virtual platforms, a situation which pulls them into obtaining what they want. This explains some care seekers’ preferences for internet channels over the advice given by physicians.
Similar cases are documented in Troein’s (2020) fieldnotes. For example, a middle-aged man with erectile dysfunction was prescribed the potency drug Viagra but was interested in something stronger. Instead of talking to physicians, he searched on the internet and found “some super pills” that could be purchased without prescriptions. In another case, a person found it “annoying” to ask for a new prescription for opioid painkillers to treat back pain because this person was mainly interested in the narcotic effects of the medicine (Troein 2020). These cases are drawn from physicians’ everyday experiences in care delivery. They are anecdotal yet indicate that some care seekers do not contact or inform physicians about their medical conditions for problems of a sensitive nature (Sugiura 2018; cf. Johnson 2019). Furthermore, they suggest that accessing medicines does not point directly to a lack of trust in care providers. To some extent, it is sensible to argue that care seekers bypass physicians to avoid being judged or to save the physical and emotional effort of persuading physicians for a prescription. Additionally, they point to the changing healthcare landscape as an element affecting care practices. The internet allows space for multiple authorities, leaving care seekers to decide whom they choose to relate to. Individual agency, the capability to act, is then enacted (Liu & Lundin 2020). This enactment is not all planned in advance by external strategies, but can be viewed as care seekers tinkering with the material resources at hand and the alternatives afforded in social structures (Schneider-Kamp & Askegaard 2020).
Theories of the materialities of things do not view medicines as fixed but as contingent to specific sociomaterial configurations. In our data, some care seekers demonstrated a clear reluctance to visit physicians to obtain medicines because they felt uncomfortable communicating their health issues. In other scenarios they felt that physicians did not take their concerns seriously or were not actively finding ways to alleviate their suffering. These people tended to seek support in virtual chat forums or purchase medicines outside the formal healthcare system. Although purchasing medicines in legal grey zones inheres risks, it has allowed care seekers to avoid healthcare paternalism and to (re)allocate trust towards anonymous self-claimed online experts. Consuming medical products is therefore not just about curing medically defined illnesses, but about managing one’s emotional state that was shaped by social norms (Humbracht, Hyun & Lundin 2016; Sugiura 2018). As mentioned earlier, in Swedish society self-care culture and health consumerism are increasingly ingrained in everyday care practices. Yet the examples presented in this section make clear that sociomaterial conditions such as the digital infrastructure and opportunities to share experiences among peers, affect how people relate to medicines and care providers. In the next section, we turn to physicians to show how they understood medicine access in grey zones and imagined a meaningful engagement with care seekers.
What Physicians Said
A statistical analysis of the Sifo survey shows that 78.5 percent of the respondents knew about the phenomenon of falsified medicines and 36.5 percent had met care seekers whom they suspected had consumed such products (Funestrand et al. 2019). These numbers imply that most physician-respondents were familiar with the spread of unsafe medicines. According to Swedish law, care providers are obligated to report any suspicious side effects of medicines to the Swedish Medical Products Agency (Swedish Medical Products Agency 2012). They are also expected to inform care seekers about risks of self-medication and for example sharing prescription drugs with others or buying medicines from unauthorized sources. Regardless of these requirements, our material suggests that physicians do not always give advice to care seekers or notify the Swedish MPA about potential cases of falsified medicines. We wondered why. The survey’s free-text comments enabled us to piece together a fuller picture.
Physician-respondents described a typical situation in which care seekers asked for an appointment due to unusual acute medical conditions. These problems were often caused by the adverse effects of medical products that care seekers had obtained through informal channels or markets abroad. One physician explained:
I’ve met several patients (…) with problems where I wasn’t sure how to diagnose [them] correctly. A patient came because [the medicine bought outside formal healthcare] caused severe problems and [the patient] got withdrawal symptoms because the drug was probably not genuine.
Another physician recounted treating people who had obtained “strange products from health food stores, but”, he added, “it is also common for people to buy illegal drugs from abroad or to travel with the purpose to shop and then take [illegal drugs] home, perhaps for their own use but also to sell to others”. Buying medicines during travel abroad was not exceptional. It has been documented that some Swedish residents buy medicines at overseas holiday destinations due to their laxer regulations on prescription medicines (Röing et al. 2020). However, while there was a tendency to assume that medicines purchased abroad could be problematic, several physicians highlighted that this assumption was not always valid. For example, one physician wrote:
Not all medicines obtained abroad are illegal or falsified. Some medicines available in other countries, such as Greece, Spain, USA, are not illegal. These countries have other therapy traditions. It has to be acknowledged.
The above quote indicates that physicians took various factors into account when they assessed whether care seekers’ symptoms might be related to poor-quality medicines. They understood that use of purportedly illicit medications could be affected by specific prescription traditions. In their view, prescribing and dispensing medicines were medical decisions in which care providers reviewed patients’ symptoms, selected a drug, and determined the strength, dosage, and the length of a treatment. They also stressed the need to consider possible risks of adverse effects and interactions with other medicines. Through such evaluations and considerations of different social and material contexts, physicians formed judgements about safe or unsafe medicine access and use. This elucidates the ambivalence physician-respondents expressed against simply categorizing medicine access as legal or illegal.
According to physician-respondents, in addition to travels abroad, another main source of exposure to problematic medicines was the internet. Those medicines mentioned by the respondents included narcotic painkillers, anabolic steroids, tranquilizers, sexual potency enhancing drugs, and antibiotics. One physician described a situation in which a person came to the clinic for acute problems but did not want to explain his illness. Finally, the physician confronted the person who “answered yes to my suspicions, and admitted having used sildenafil-like drugs [potency-enhancing drugs] bought on the internet”. This incident resonates with some care seekers’ statements about online shopping alternatives presented in the previous section. Additionally, physician-respondents speculated that care seekers turned to various online chatrooms for information about medicines. One physician commented:
An increasing problem is the behaviour of especially young people who may be on Flashback where they participate in various Darknet discussion groups, different websites, etc. and then they order drugs from everywhere.
Similarly, another physician wrote “it is obvious that [young people] experiment without reflecting on the consequences… and the descriptions [of the drugs] on the websites are often trivial, [it is] easy to order…”. From the Sifo survey material, it is hard to tell from where these speculations are drawn. However, given that nearly 90 percent of physician-respondents stated to have read about the issue of falsified medicines from the media, we can well reason that physicians’ understanding of digital health consumption is influenced by media portraits of health consumers. It means that media coverage plays a role in physicians’ imagining of care seekers and their consumption behaviours. Reading between the lines, care seekers’ ability to consume medicines responsibly is questioned by the physician-respondents.
Dealing with medicine access in grey zones appeared to be a practical challenge for the physicians in our survey. In an open-ended question asking for their responses to cases of potentially unsafe medicine access, we identified a great deal of uncertainty. Some simply replied “I am not sure”. One physician wrote: “I suppose it needs to be reported to the Swedish Medical Products Agency”. Another stated: “I met patients who ordered antibiotics via the net from a foreign supplier, but as far as I know it is not illegal, and so I didn’t act”. Others sounded more familiar with the regulations and commented that they would “first confront the patient, then report [it] to the medical authority”. These diversified responses suggest a shared understanding among physician-respondents about their professional duty to advise care seekers against unsafe medicine consumption. Nearly all stated that they wanted more training and information on the subject of falsified medicines. Certainly, information campaigns could be one way forward. Nevertheless, as pointed out by one physician and repeated in other comments, a pertinent issue is how “to get the patients to show the drug and tell you how they got it”.
Medical encounters can be characterized as a type of expert services (Azzari et al. 2021). They entail asymmetric knowledge and power between care providers and care seekers. However, they are also similar to other social encounters, if one considers them to be a site where “complex patterns of knowledge and practice are operationalized and negotiated” (May 2010: 132). In physician-respondents’ reasoning about safe versus unsafe and legal versus illegal medicine access, it becomes apparent that professional judgement is not pre-inscribed or ready to use. Instead, this judgement goes through constant pondering about particular social and material relations before medical decisions are formed. It is in this regard that the materialities of medicine as processual and emergent become visible. A key element in these negotiations, however, is deemed difficult to grasp by physician-respondents. Quoting one respondent, this is the “scenario” wherein people decide from where and how to access medicines. Many respondents raised the concern of visibility, since “those buying from informal or illegal channels probably don’t come to us”. In the next section, we further explore these challenges by situating physician–patient encounters in societal transitions and healthcare models.
Treatment as Service
The last couple of decades of Swedish healthcare have been characterized by increasingly digitalized services and an emphasis on active patient participation. Contemporary Sweden is a highly individualized society in which the welfare state has largely been replaced by the idea of a consumer society (Fotaki 2011). Many of our physician-respondents perceived their duty as “understand[ing] a patient’s medical history and to mak[ing] diagnoses that lead to treatment”. Yet treatment could prove difficult for physicians to provide, due to “sometimes long waiting times to get an appointment with your GP (---) and then they’re off to other places. There are lots of alternatives today.” One physician expressed similar concerns:
What is really worrying is that in recent years there are so many [private] players online – the range is huge and no wonder it’s difficult to keep track of who is serious, it’s frightening that an unregulated online pharma market exists with both potent and ineffective medicines. (…) There are so many tempting offers to lose weight or build muscle and so on.
This quote indicates physician-respondents’ awareness of the pressures posed by the liberal market structure, particularly in the sense that emerging alternatives might draw people away from formal healthcare systems. Our empirical materials reflect that physicians are often seen as medical tools whose expertise is endowed by their institutional authority in writing prescriptions. This is evident in a comment by a lay respondent: “a visit to the physician is needed to get a prescription, but I always prepare beforehand and then I ask for the medicine I want”. Equally, another lay respondent revealed “it is better to look for alternative ways to get medicines and sometimes I buy online because it’s simply too tiresome to persuade [the physicians] to get it prescribed”.
Looking for alternative medicines is far from a newly discovered phenomenon. Alternative care strategies are well-established and deeply rooted in previous historical times (Lock & Nguyen 2010; Waisse & Eklöf 2019). In the folklife archives in Sweden, a multitude of narratives were collected about strategies for seeking cures from folk medicines for infertility, protection against life-threatening injuries, premature death and the like in the older peasant society (Tillhagen 1958). Over the past few decades, however, the internet and increasing globalization of information and markets have made visible previously unknown opportunities (Lundin, Torkelson & Petersen 2016). Purchases from global pharmaceutical markets may represent, as a lay respondent wrote, “voting with [one’s] feet” due to the large price differences among different jurisdictions. The person in question “regularly uses migraine drugs which are relatively expensive in Sweden and the same substance I can buy at a fraction of the price in Bangkok”. On the surface, this sounds a complaint about economic costs. Deep down, it may express a desire for an affective relationship with care providers, one in which the state and healthcare system would take care of those in need. Some of our lay respondents felt they had to seek care from alternative arenas “if the medical profession deteriorates further and you do not get any help but are sent back and forth and you are ignored”. Bricolaging statements of both physicians and care seekers, our material shows that the frictions experienced by both parties in care service encounters do not derive from diverging views on diversified medicine access. In fact, both parties are well aware of the existence of alternatives. Physician-patient encounters are geographically confined to the consultation rooms, but these are meeting points where various interpretations of health policies and different ideas of what care services should look like collide.
When market-adapted structures shape the healthcare arena, physician-patient meetings are transformed into service encounters. Studies show that care seekers become informed health consumers and learn to mobilize various resources to manage their health (Liu & Lundin 2020; Phillimore et al. 2019). Medicines, as tangible objects passing from hand to hand and moving across different markets, play a central role in the pharmaceuticalization of health (Fox & Ward 2008; Johnson 2019). For this reason, providing medical care involves more than making diagnoses or writing prescriptions. Our material on care seekers implies that if certain expectations are not met, for example if care seekers do not feel they are being treated with respect, they may look for alternative markets, virtual or physical, with alternative expertise, where falsified medicines may circulate. Accessing medicines in grey zones, thus, is less about rebelling against medical authorities than a negotiation of power involving “the relational manoeuvring of users and technologies in practices” (Nielsen & Langstrup 2018: 264). This relational manoeuvring applies to both care seekers and physicians because decisions and evaluations on appropriate medicine access are not emotionless or purely biomedical, but co-evolve with elements such as biomedical advancements and digital infrastructures. To avoid situations where care providers do not ask and care seekers do not tell, we argue that medicines should be recognized as social objects (Appadurai 1986) to better approach patient-centred care.
Conclusion: The Importance of Curiosity
Our two-fold aim has been, firstly, to advance sociocultural analyses that investigate relationships between physicians and care seekers, and, secondly, to contribute knowledge that can be implemented in healthcare.
Our analyses have demonstrated that the relationships between care providers and care seekers are affected by societal changes, including an emphasis on individual responsibility and consumer choice, but also technological changes such as the digital infrastructure. Accordingly, care services and medicine consumption patterns are undergoing change. Whereas healthcare models emphasize active patient participation, our material indicates that paternalism in physician–patient encounters remains. Care seekers in our study acknowledged physicians’ expertise but they also expected an engaging and affective relationship with care providers. Physician-respondents rarely reflected on paternalism, but voiced uncertainties on whether care seekers were able to make responsible choices. These medical professionals also felt challenged by emerging alternatives in globalized and liberalized pharmaceutical markets. As more access and purchasing channels in legal grey zones become available and accessible, physicians are at the risk of being instrumentalized as simply medicine prescribers. Drawing on Appadurai’s (1986) idea that objects have a social life of their own, and Ingold’s (2012) notion of materialities as negotiated, we propose conceptualizing physician–patient encounters as sociomaterially embedded, as encounters where diverse knowledge systems are communicated into an agreed-on treatment scheme. Diverging views held by physicians and care seekers do not necessarily position professional knowledge in opposition to lay knowledge. Rather, these differences are partly shaped and channelled by a changing healthcare landscape that allows competing expert claims. Examining physician–patient relationships then requires situating care providers’ and care seekers’ ideas and perceptions in a broader societal context.
This article has empirically demonstrated the importance of highlighting the materialities of medicines as negotiated and fluid to understand physician–patient encounters. In order to engage with care seekers in a meaningful way, we suggest that healthcare practitioners and policymakers take as their point of departure both the biological body and the sociomaterially conditioned practices of care. For care providers, confronting care seekers with sensitive questions without offending them is not easy. Linking back to Seeberger (2010) as quoted in the beginning of this article, it requires shameless curiosity about care seekers’ medical needs as well as their expectations of care services. It also calls for respect, consideration, and well-honed communication skills. Strategies are needed to implement already-existing theoretical models such as patient-centred care that considers care seekers’ desires, emotions, social circumstances, and lifestyles (Olin Lauritzen & Sachs 2001). To counteract the risk of people being exposed to unsafe medicines, physicians could perhaps inquire: What kind of medicines have you taken, where was the medicine purchased, and not least, why have you purchased the products that are suspected to have caused the trouble?
Notes
- https://ec.europa.eu/health/human-use/eu-logo_en (accessed November 23, 2022). [^]
- Our research has been approved by the Swedish Regional Ethical Review Board (2016-238, 2019-03501 & 2019-02226). [^]
Acknowledgements
This work was supported by the Erik Philip-Sörensen Foundation 2017 [H2016-015], VINNOVA [VLU14-1006, V16-0307], the Marcus and Amalia Wallenberg Foundation 2020 [2020.0004], the LMK-Foundation and the STIAS Wallenberg Research Centre, 10 Marais Road, Stellenbosch, South Africa. We thank the participants in the study.
Competing Interests
The authors have no competing interests to declare.
References
Literature
Appadurai, Arjun (ed.) 1986: The Social Life of Things: Commodities in Cultural Perspective. Cambridge: Cambridge University Press. DOI: https://doi.org/10.1017/CBO9780511819582
Attaran, Amir 2015: Stopping Murder by Medicine: Introducing the Model Law on Medicine Crime. The American Journal of Tropical Medicine and Hygiene 92(6): 127–132. DOI: https://doi.org/10.4269/ajtmh.15-0154
Azzari, Courtney Nations, Laurel Anderson, Martin Mende, Josephine Go Jefferies, Hilary Downey, Amy L. Ostrom & Jelena Spanjol 2021: Consumers on the Job: Contextualization Crafting in Expert Services. Journal of Service Research 24(4): 520–541. DOI: https://doi.org/10.1177/10946705211012474
Baxerres, Carine & Jean-Yves Le Hesran 2011: Where do Pharmaceuticals on the Market Originate? An Analysis of the Informal Drug Supply in Cotonou, Benin. Social Science & Medicine 73(8): 1249–1256. DOI: https://doi.org/10.1016/j.socscimed.2011.03.050
Burrell, Jenna 2009: The Field Site as a Network: A Strategy for Locating Ethnographic Research. Field Methods 21(2): 181–199. DOI: https://doi.org/10.1177/1525822X08329699
Coderey, Celine 2019: Immortal Medicine: Understanding the Resilience of Burmese Alchemic Practice. Medical Anthropology: Cross Cultural Studies in Health and Illness 38(4): 412–424. DOI: https://doi.org/10.1080/01459740.2018.1550756
Derksen, Frans, Jozien Bensing & Antoine Lagro-Janssen 2013: Effectiveness of Empathy in General Practice: A Systematic Review. British Journal of General Practice 63(606): e76. DOI: https://doi.org/10.3399/bjgp13X660814
Ehn, Billy, Orvar Löfgren & Richard R. Wilk 2016: Exploring Everyday Life: Strategies for Ethnography and Cultural Analysis. Lanham: Rowman & Littlefield.
Epstein, Ronald M. & Richard L. Street 2011: The Values and Value of Patient-Centered Care. The Annals of Family Medicine 9(2): 100–103. DOI: https://doi.org/10.1370/afm.1239
Fioretos, Ingrid, Kristofer Hansson & Gabriella Nilsson 2013: Vårdmöten: Kulturanalytiska perspektiv på möten inom vården [Health care encounters: Culture analytical perspectives on encounters within health care]. Lund: Studentlitteratur.
Fotaki, Marianna 2011: Towards Developing New Partnerships in Public Services: Users as Consumers, Citizens and/or Co-producers in Health and Social Care in England and Sweden. Public Administration 89(3): 933–955. DOI: https://doi.org/10.1111/j.1467-9299.2010.01879.x
Fox, Nick J. & Katie J. Ward 2008: Pharma in the bedroom … and the kitchen: The Pharmaceuticalisation of Daily Life. Sociology of Health & Illness 30(6): 856–868. DOI: https://doi.org/10.1111/j.1467-9566.2008.01114.x
Funestrand, Henrik, Rui Liu, Susanne Lundin & Margareta Troein 2019: Substandard and Falsified Medical Products are a Global Public Health Threat: A Pilot Survey of Awareness among Physicians in Sweden. Journal of Public Health 41(1): e95–e102. DOI: https://doi.org/10.1093/pubmed/fdy092
Gabe, Jonathan, Kirsten Harley & Michael Calnan 2015: Healthcare Choice: Discourses, Perceptions, Experiences and Practices. Current Sociology 63(5): 623–635. DOI: https://doi.org/10.1177/0011392115590061
Gabriels, Katleen & Tania Moerenhout 2018: Exploring Entertainment Medicine and Professionalization of Self-care: Interview Study among Doctors on the Potential Effects of Digital Self-tracking. Journal of Medical Internet Research 20(1): e10. DOI: https://doi.org/10.2196/jmir.8040
Hall, Alexandra & Georgios A. Antonopoulos 2016: Fake Meds Online: The Internet and the Transnational Market in Illicit Pharmaceuticals. Basingstoke: Palgrave Macmillan.
Hamill, Heather, Kate Hampshire, Simon Mariwah, Daniel Amoako-Sakyi, Abigail Kyei & Michele Castelli 2019: Managing Uncertainty in Medicine Quality in Ghana: The Cognitive and Affective Basis of Trust in a High-risk, Low-regulation Context. Social Science & Medicine 234: 112369. DOI: https://doi.org/10.1016/j.socscimed.2019.112369
Hamilton, William L., Cormac Doyle, Mycroft Halliwell-Ewen & Gabriel Lambert 2016: Public Health Interventions to Protect against Falsified Medicines: A Systematic Review of International, National and Local Policies. Health Policy and Planning 31(10): 1448–1466. DOI: https://doi.org/10.1093/heapol/czw062
Hardon, Anita & E. Vicente Sanabria 2017: Fluid Drugs: Revisiting the Anthropology of Pharmaceuticals. Annual Review of Anthropology 46(1): 117–132. DOI: https://doi.org/10.1146/annurev-anthro-102116-041539
Henderson, Sarah & Alan R. Petersen 2002: Consuming Health: The Commodification of Health Care. London: Routledge. DOI: https://doi.org/10.1046/j.1365-2524.2002.03843.x
Hornberger Julia 2019: Who is the fake one now? Questions of Quackery, Worldliness and Legitimacy. Critical Public Health 29(4): 484–493. DOI: https://doi.org/10.1080/09581596.2019.1602719
Humbracht, Michael, Insoo Hyun & Susanne Lundin 2016: Managing Hope and Spiritual Distress: The Centrality of the Doctor–Patient Relationship Combatting Stem Cell Travel. In: Erik Malmkvist & Kristin Zeiler (eds.), Bodily Exchanges, Bioethics and Border Crossing: Perspectives on Giving, Selling and Sharing bodies. Abingdon, Oxon: Routledge, 153–168.
Ingold, Tim 2012: Toward an Ecology of Materials. Annual Review of Anthropology 41: 427–442. DOI: https://doi.org/10.1146/annurev-anthro-081309-145920
Irvine, Rob 2002: Fabricating “Health Consumer” in Health Care Politics. In: Sarah Henderson & Alan Petersen (eds.), Consuming Health: The Commodification of Health Care. London: Routledge.
Johnson, Ericka 2019: Refracting through Technologies: Bodies, Medical Technologies and Norms. London: Routledge. DOI: https://doi.org/10.4324/9781315122274
Kingori, Patricia & René Gerrets 2019: Why the Pseudo Matters to Global Health. Critical Public Health 29(4): 379–389. DOI: https://doi.org/10.1080/09581596.2019.1605155
Kleinman, Arthur 2013: From Illness as Culture to Caregiving as Moral Experience. New England Journal of Medicine 368(15): 1376–1377. DOI: https://doi.org/10.1056/NEJMp1300678
Krieg, Lisa Jenny, Moritz Berning & Anita Hardon 2017: Anthropology with Algorithms? An Exploration of Online Drug Knowledge and Using Digital Methods. Medicine Anthropology Theory 4(3): 21–52. DOI: https://doi.org/10.17157/mat.4.3.458
Lavorgna, Anita 2021: Information Pollution as Social Harm: Investigating the Digital Drift of Medical Misinformation in a Time of Crisis. Bingley, UK: Emerald Publishing Limited. DOI: https://doi.org/10.1108/9781800715219
Liu, Rui & Susanne Lundin 2016: Falsified Medicines: Literature Review. Working Papers in Medical Humanities 2(1): 1–25.
Liu, Rui & Susanne Lundin 2020: Medicines in the Grey Market: A Sociocultural Analysis of Individual Agency. In: Kristofer Hansson & Rachel Irwin (eds.), Movement of Knowledge: Medical Humanities Perspective on Medicine, Science, and Experience. Lund: Nordic Academic Press, 229–255. DOI: https://doi.org/10.21525/kriterium.24.j
Lock, Margaret M. & Vinh-Kim Nguyen 2010: An Anthropology of Biomedicine. Chichester: Wiley-Blackwell.
Lundin, Susanne & Markus Idvall 2003: Attitudes of Swedes to Marginal Donors and Xenotransplantation. Journal of Medical Ethics 29(3): 186–192. DOI: https://doi.org/10.1136/jme.29.3.186
Lundin, Susanne & Rui Liu 2019: “Where and how do you buy medicines?” A Pilot Survey of Consumption Strategies among the Public in Sweden. Journal of Public Health 42(3): e268–e271. DOI: https://doi.org/10.1093/pubmed/fdz075
Lundin, Susanne, Eva Torkelson & Marsanna Petersen 2016: “With this disease, you take whatever chances there are”: A Study on Socio-cultural and Psychological Aspects of Experiments Regarding Huntington’s Disease. Open Journal of Medical Psychology 5(4): 72–87. DOI: https://doi.org/10.4236/ojmp.2016.54009
Lupton, Deborah 2014: The Commodification of Patient Opinion: The Digital Patient Experience Economy in the Age of Big Data. Sociology of Health & Illness 36(6): 856–869. DOI: https://doi.org/10.1111/1467-9566.12109
Lupton, Deborah 2018: Digital Health: Critical and Cross-disciplinary Perspectives. Milton Park, Abingdon, Oxon & New York, NY: Routledge. DOI: https://doi.org/10.4324/9781315648835
Mackey, Tim K. & Gaurvika Nayyar 2016: Digital Danger: A Review of the Global Public Health, Patient Safety and Cybersecurity Threats Posed by Illicit Online Pharmacies. British Medical Bulletin 118(1): 110–126. DOI: https://doi.org/10.1093/bmb/ldw016
Marcus, Georg 1995: Ethnography in/of the World System: The Emergence of Multi-sited Ethnography. Annual Review of Anthropology 24(1): 95117. DOI: https://doi.org/10.1146/annurev.an.24.100195.000523
Maslen, Sarah & Deborah Lupton 2019: “Keeping it real”: Women’s Enactments of Lay Health Knowledges and Expertise on Facebook. Sociology of Health & Illness 41(8): 1637–1651. DOI: https://doi.org/10.1111/1467-9566.12982
May, Carl 2010: Retheorizing the Clinical Encounter: Normalization Processes and the Corporate Ecologies of Care. In: Graham Scambler & Sasha Scambler (eds.), New Directions in the Sociology of Chronic and Disabling Conditions: Assaults on the Lifeworld. London: Palgrave Macmillan UK, 129–145. DOI: https://doi.org/10.1057/9780230297432_7
Michailakis, Dimitris & Werner Schirmer 2010: Agents of their Health? How the Swedish Welfare State Introduces Expectations of Individual Responsibility. Sociology of Health & Illness 32(6): 930–947. DOI: https://doi.org/10.1111/j.1467-9566.2010.01262.x
Mol, Annemarie 2008: The Logic of Care: Health and the Problem of Patient Choice. Abingdon, Oxon: Routledge.
Naughton, Bernard 2019: Medicine Authentication Technology: A Quantitative Study of Incorrect Quarantine, Average Response Times and Offline Issues in a Hospital Setting. BMJ Open 9(2): e026619. DOI: https://doi.org/10.1136/bmjopen-2018-026619
Nielsen, Karen Dam & Henriette Langstrup 2018: Tactics of Material Participation: How Patients Shape their Engagement through E-health. Social Studies of Science 48(2): 259–282. DOI: https://doi.org/10.1177/0306312718769156
Nordstrom, Carolyn 2007: Global Outlaws: Crime, Money, and Power in the Contemporary World. Berkeley: University of California Press.
Olin Lauritzen, Sonja & Lisbeth Sachs 2001: Normality, Risk and the Future: Implicit Communication of Threat in Health Surveillance. Sociology of Health and Illness 23(4): 497–516. DOI: https://doi.org/10.1111/1467-9566.00262
Phillimore, Jenny, Hannah Bradby, Michi Knecht, Beatriz Padilla & Simon Pemberton 2019: Bricolage as Conceptual Tool for Understanding Access to Healthcare in Superdiverse Populations. Social Theory & Health 17(2): 231–252. DOI: https://doi.org/10.1057/s41285-018-0075-4
Quet, Mathieu 2017: Values in Motion: Anti-counterfeiting Measures and the Securitization of Pharmaceutical Flows. Journal of Cultural Economy 10(2): 150–162. DOI: https://doi.org/10.1080/17530350.2016.1258001
Röing, Marta, Ingeborg Björkman, Jaran Eriksen & Cecilia Stålsby Lundborg 2020: The Challenges of Implementing National Policies to Contain Antibiotic Resistance in Swedish Healthcare: A Qualitative Study of Perceptions among Healthcare Professionals. PLoS ONE 15(5): e0233236. DOI: https://doi.org/10.1371/journal.pone.0233236
Sachs, Lisbeth 2006: Effects of Magic Come in from the Cold: Pictorial Evidence of Placebo Effect. Scandinavian Journal of Public Health 34(4): 342–345. DOI: https://doi.org/10.1080/14034940600646010
Schneider-Kamp, Anna & Soren Askegaard 2020: Putting Patients into the Centre: Patient Empowerment in Everyday Health Practices. Health 24(6): 625–645. DOI: https://doi.org/10.1177/1363459319831343
Seeberger, Astrid 2010: Den skamlösa nyfikenheten [The shameless curiosity]. Stockholm: Weyler förlag.
Sugiura, Lisa 2018: Respectable Deviance and Purchasing Medicine Online: Opportunities and Risks for Consumers. Cham: Springer Nature. DOI: https://doi.org/10.1007/978-3-319-74485-8
Teddlie, Charles & Abbas Tashakkori 2012: Common “Core” Characteristics of Mixed Methods Research: A Review of Critical Issues and Call for Greater Convergence. American Behavioral Scientist 56(6): 774–788. DOI: https://doi.org/10.1177/0002764211433795
Tillhagen, Carl-Herman 1958: Folklig läkekonst [Folk medicine]. Nordiska museet.
Wachtler, Caroline, Annika Brorsson & Margareta Troein 2006: Meeting and Treating Cultural Difference in Primary Care: A Qualitative Interview Study. Family Practice 23(1): 111–115. DOI: https://doi.org/10.1093/fampra/cmi086
Waisse, Silvia & Motzi Eklöf 2019: Homeopathy in Sweden and Brazil, 1880–1930. Lychnos: Årsbok för idé-och lärdomshistoria, 175–197.
Whyte, Susan Reynolds, Sjaak van der Geest & Anita Hardon 2002: Social Lives of Medicines. Cambridge, UK: Cambridge University Press.
Wiszmeg, Andréa, Susanne Lundin, Eva Torkelson, Niclas Hagen & Cecilia Lundberg 2012: Difficult Questions and Ambivalent Answers on Genetic Testing. Culture Unbound 4(3): 463–480. DOI: https://doi.org/10.3384/cu.2000.1525.124463
World Health Organization 2017: A Study on the Public Health and Socioeconomic Impact of Substandard and Falsified Medical Products. Geneva.
Internet Sources
Interpol 2017: Millions of Medicines Seized in Largest Interpol Operation against Illicit Online Pharmacies, https://www.interpol.int/en/News-and-Events/News/2017/Millions-of-medicines-seized-in-largest-INTERPOL-operation-against-illicit-online-pharmacies (accessed June 7, 2022).
SOU 1997: 154. Patienten har rätt [The patient is right], https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/1997/11/sou-1997154/ (accessed September 2, 2022).
Statista 2020: Daily Usage of Digital and Online Medica in Sweden 2020, https://www.statista.com/statistics/438356/daily-usage-of-digital-and-online-media-in-sweden-by-medium/#statisticContainer (accessed June 8, 2022).
Swedish Medical Products Agency 2012: LVFS 2012:14, https://www.lakemedelsverket.se/sv/lagar-och-regler/foreskrifter/2012-14 (accessed June 8, 2022).
Field Diaries
Liu, Rui 2019: Non-participant observations on Swedish chat forums.
Liu, Rui & Susanne Lundin 2017: Participant observations at the Swedish customs clearance office at Arlanda International Airport, Stockholm.
Lundin, Susanne 2019: Non-participant observations on Swedish chat forums.
Troein, Margareta 2020: Participant observations at a healthcare centre.
Rui Liu is a PhD candidate at the Department of Service Management and Service Studies, Lund University, Sweden. She studies medicine consumption and health care services. A recent publication is Care in the Air? An Ethnographic Study of Swedish Pharmacies, in Journal of Material Culture (online first https://doi.org/10.1177/13591835221133289).
Susanne Lundin is professor at the Department of Arts and Cultural Sciences, Lund University, Sweden, and research fellow at Stellenbosch Institute of Advanced Study (STIAS), Wallenberg Research Centre at Stellenbosch University, South Africa. She has published widely on the body in health and illness, medical technologies, and social change. Her interest also concerns medical treatments and medicines in the global black market.
Talieh Mirsalehi is a PhD candidate at the Department of Arts and Cultural Sciences, Lund University, Sweden. She studies the interconnections between migration, body, and care seeking practices. Her latest publication appears in Ethnologia Scandinavica 2021, with the title “We only drink water here”: An Ethnological Approach to the Liminality of Childhood Migration, Health Narratives, and Negotiation of Belonging in Sweden.
(talieh.mirsalehi@kultur.lu.se)
Margareta Troein is professor emerita at the Department of Clinical Sciences, Malmö, and Family Medicine, Lund University, Sweden. Her research is about physician education, sustainable working environment at primary care, and falsified medicines.